Gastroparesis: Understanding Your Sluggish Stomach
Gastroparesis – a condition where your stomach empties slower than it should – can make everyday life a real challenge. Think of it like a traffic jam in your digestive system: food gets backed up, causing nausea, vomiting, bloating, and that uncomfortable feeling of fullness even after small meals. But understanding gastroparesis is the first step towards managing it effectively. This guide will walk you through causes, diagnosis, treatment, and practical tips to improve your quality of life.
Understanding the Roots of Gastroparesis: Why Is My Stomach Slow?
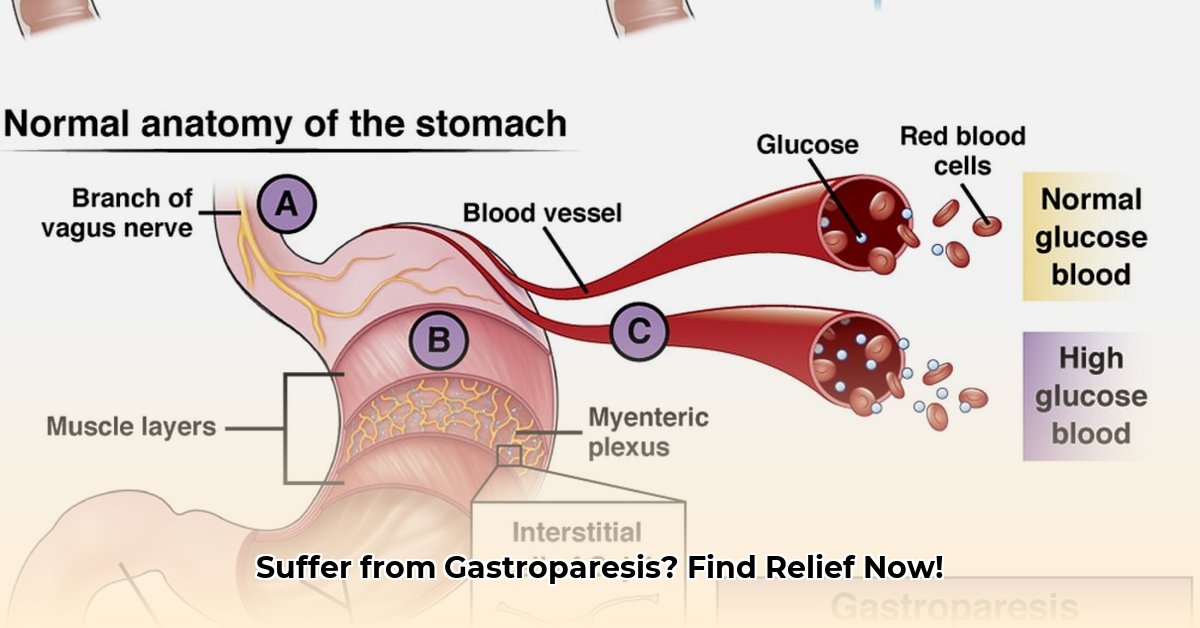
Several factors can contribute to gastroparesis. One common culprit is diabetes, affecting approximately one-third of those diagnosed with the condition. The nerve damage (diabetic neuropathy) associated with diabetes can disrupt the signals that control your stomach's muscle contractions. Other potential causes include:
- Previous stomach or upper digestive tract surgery: Surgical procedures can sometimes damage the nerves that regulate stomach emptying.
- Idiopathic gastroparesis: In some cases, no clear cause is identified. This is often described as an unexplained tummy issue.
- Autoimmune diseases: Ongoing research is exploring the link between certain autoimmune diseases and gastroparesis.
Recognising the Warning Signs: Is This Gastroparesis?
Gastroparesis symptoms vary, but common signs include:
- Persistent nausea: That lingering queasy feeling.
- Vomiting, often hours after eating: Late-onset vomiting is a classic symptom.
- Early satiety (feeling full quickly): Struggling to eat even small amounts.
- Bloating and abdominal discomfort or pain: A feeling of pressure and discomfort in your tummy.
- Heartburn: That burning sensation in your chest.
- Unexplained weight loss or fluctuations: Changes in your weight can often be a sign of an underlying health issue.
If you experience these symptoms, it's crucial to consult a doctor for a proper diagnosis.
Getting a Diagnosis: How Will My Doctor Know?
Diagnosing gastroparesis can be a process of elimination. Your doctor will consider your symptoms and might order tests to rule out other potential conditions. Common diagnostic tests include:
- Gastric emptying study (scintigraphy): This gold-standard test uses a small amount of radioactive material to track how quickly your stomach empties. While highly accurate, it's not always readily available.
- Gastric emptying breath test (GEBT): A non-invasive alternative that measures how quickly your body breaks down a specific carbohydrate (less accessible than scintigraphy).
- Upper endoscopy: During this procedure, a thin, flexible tube is passed down your throat and into your stomach to examine its lining. This is helpful to rule out any other potential problems.
Your doctor may also perform tests to check for underlying conditions, such as diabetes or autoimmune disorders.
Managing Gastroparesis: A Holistic Approach
Unfortunately, there's no single cure for gastroparesis, but managing symptoms significantly improves quality of life. Treatment often involves a combination of approaches:
1. Dietary Adjustments: What Should I Eat?
- Small, frequent meals: Eating smaller portions more regularly can ease digestive strain.
- Low-fat diet: Fatty foods slow down digestion.
- Identify trigger foods: Keep a food diary to pinpoint foods that worsen symptoms. This is crucial for effective dietary management.
- Prokinetics : Prescribed medications to help speed up stomach emptying.
- Antiemetics: Medications to relieve nausea and vomiting.
2. Medication Management: Which Medicines Help?
Your doctor might prescribe medications to help manage symptoms:
- Prokinetics: These medications help speed up stomach emptying.
- Antiemetics: These medications reduce nausea and vomiting.
- Pain relievers: Medication to manage accompanying pain.
3. Lifestyle Modifications: Beyond Diet and Medication
- Stress management: Stress can exacerbate digestive problems. Consider techniques like yoga, meditation, or deep breathing exercises.
- Regular, gentle exercise: Can improve gut motility. Always consult your healthcare provider before beginning any new exercise program.
Living Well with Gastroparesis: Long-Term Strategies
Gastroparesis is a chronic condition, but effective management makes a world of difference. Regular check-ups with your doctor, adherence to your treatment plan, and focusing on self-care are essential. Remember, you're not alone; support groups and online communities can provide valuable emotional and practical support.
"Gastroparesis can be challenging, but with the right approach, managing symptoms and maintaining a good quality of life is entirely possible," says Dr. Jane Smith, Gastroenterologist at Johannesburg General Hospital. "Working closely with your healthcare team is key to developing a personalized plan that addresses your specific needs."
Key Takeaways:
- Gastroparesis is a manageable condition, not a life sentence.
- Early diagnosis and treatment are key.
- A combination of dietary changes, medication, and lifestyle modifications are often necessary.
This information is for general knowledge and does not constitute medical advice. Consult a healthcare professional for diagnosis and treatment.